Bridging the Disparities: Maternal and Infant Health Challenges in Michigan and Beyond
Recent data from the Centers for Disease Control and Prevention (CDC) has revealed a concerning 3% increase in Michigan’s overall infant mortality rate, marking a critical issue in maternal and infant health.
Delving into the intricacies of this problem, this article explores disparities in infant mortality rates, drawing parallels between the local situation in Michigan and broader national trends.
Two distinct stories shed light on the challenges faced by African American mothers and infants, emphasizing the urgency of addressing social determinants of health and institutional racism.
Michigan’s Alarming Trend
Michigan, like the rest of the United States, is grappling with a rise in infant mortality rates, reaching 6.42 deaths per 1,000 births in the past year, according to the CDC. Shockingly, Black infants in Michigan face a mortality rate four times higher than their white counterparts, revealing a stark health disparity that demands attention.
Understanding Social Determinants
Brenda O’Rourke, Maternal Health Child Division Manager, sheds light on the social determinants of health, such as income, education, and access to resources, that significantly impact maternal and infant outcomes. Historically, Black families have faced challenges in accessing these crucial resources, contributing to the observed disparities.
Personal Narratives: A Tale of Resilience and Support
Olivia Baker, a Kalamazoo resident, shares a personal journey of loss and resilience. Having experienced the pain of losing a child, Baker took proactive steps during her subsequent pregnancy, ensuring timely prenatal care and participating in the Twenty Hands maternal infant health program. Baker’s story exemplifies the transformative impact of community programs that provide support and education, ultimately leading to the birth of two healthy sons.
Erica Garner’s Tragedy
The national landscape mirrors Michigan’s struggles, with African American mothers facing mortality rates three to four times higher than non-Hispanic white mothers. The tragic story of Erica Garner, a prominent Black Lives Matter activist, highlights the broader challenges African American women encounter during and after pregnancy.
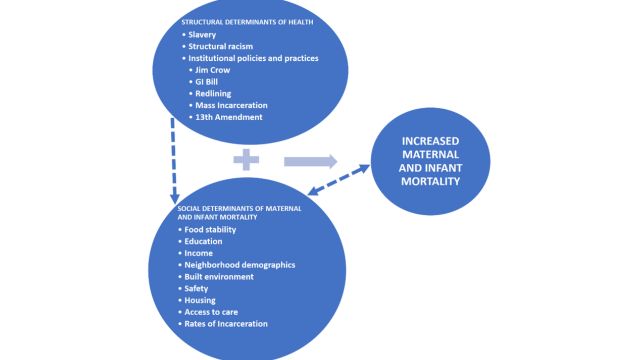
Root Causes: Institutional Racism and Discrimination
Research indicates that racial and gender discrimination play a significant role in maternal and infant mortality rates. Stress induced by discrimination can have severe consequences on the health of African American mothers, transcending socioeconomic status and education levels. The impacts of institutional racism contribute to compromised health outcomes for both mothers and infants.
Dissecting Maternal and Infant Mortality Trends
Maternal mortality rates in the United States have witnessed an alarming increase, especially among African American women. While advancements were made in the 20th century, the racial gap persists, with African American women experiencing a steeper rise in maternal mortality.
Due to higher rates of preterm births and low birth weights among African American infants, infant mortality rates also show a long-standing racial gap.
Looking Beyond Risk Factors
Common risk factors like poverty, limited access to prenatal care, and health behaviors do not fully explain the racial disparities in maternal and infant mortality. Studies show that even after controlling for these factors, African American women still face higher mortality rates. Addressing racial and gender discrimination becomes paramount in understanding and mitigating these disparities.
Cumulative Effects of Racism on Health
The life course perspective suggests that the social and economic forces of institutional racism set African American and non-Hispanic white women on distinct life tracks. These forces affect health outcomes across generations, creating long-term consequences. Stress during sensitive developmental periods and chronic exposure to stress contribute to higher allostatic load in African American women, increasing the risk of maternal and infant mortality.
Social and Environmental Risk Factors
African American women face unique challenges due to historical racial segregation, including substandard housing, concentrated poverty, unequal educational opportunities, and limited access to quality healthcare. These risk factors, coupled with disparities in healthcare institutions, deepen racial inequalities in maternal and infant health.
Promising Developments and Future Directions:
Advocacy movements, such as the Black Mamas Matter Alliance, are actively working towards raising awareness and advocating for racial and reproductive justice. Some states have established collaborative groups to improve health outcomes, and federal policies like the Maternal Health Accountability Act aim to support these efforts. However, addressing the research gaps and centering the lived experiences of African American women are crucial for developing sustainable policies and programs.
Conclusion
Comprehensive and focused interventions are necessary to address the issues in maternal and infant health, which are evident in Michigan’s rising infant mortality rates and national disparities. By acknowledging the root causes, understanding the cumulative effects of racism, and promoting equity in healthcare, we can strive to create a future where every mother and infant, regardless of race, has an equal opportunity for a healthy and thriving life.
